Understanding Low BMI Bariatric Surgery
Considering weight-loss surgery despite a relatively low BMI? This comprehensive guide clarifies the complexities of this procedure, detailing eligibility, surgical options, risks, recovery, long-term care, and financial considerations. It's designed for potential patients, surgeons, and insurance providers alike.
Eligibility Criteria: Beyond the BMI Number
While a high BMI often warrants bariatric surgery, a lower BMI doesn't automatically disqualify individuals. Serious obesity-related health conditions, such as type 2 diabetes, severe sleep apnea, or debilitating acid reflux, can indicate a need for surgical intervention, even with a moderate BMI. Dr. Anya Sharma, MD, a leading bariatric surgeon at the University of California, San Francisco, emphasizes, "BMI is a valuable metric, but it's not the only factor. We consider the totality of the patient's health, including comorbidities and their impact on quality of life." A comprehensive evaluation, including psychological assessments, is crucial to determine suitability and overall preparedness for the significant lifestyle changes required. This helps ensure both physical and mental readiness for surgery and the commitment to long-term health management.
Types of Bariatric Surgery: A Detailed Overview
Several weight-loss procedures offer diverse mechanisms. Let's explore the most common:
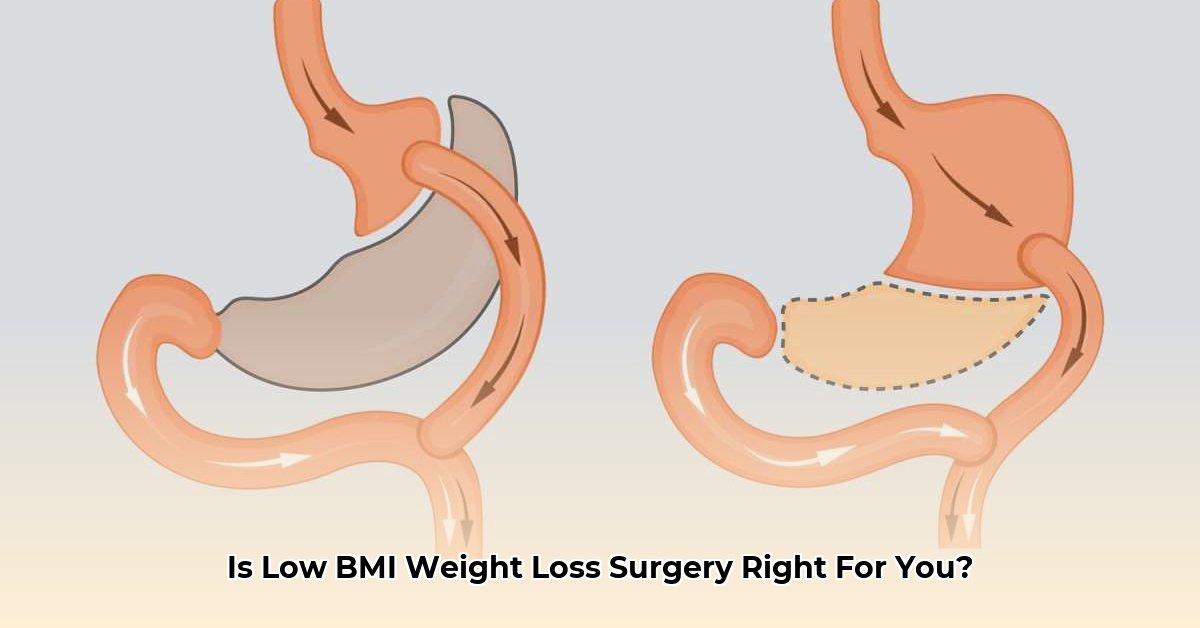
Roux-en-Y Gastric Bypass (RYGB): This procedure alters the digestive tract, reducing calorie and nutrient absorption. While highly effective in weight loss, it carries a higher risk of nutrient deficiencies and requires lifelong supplementation. (Illustration of RYGB would be beneficial here)
Sleeve Gastrectomy (SG): This restrictive procedure removes a significant portion of the stomach, reducing its capacity and promoting satiety. It generally offers a less complex recovery than RYGB. (Illustration of sleeve gastrectomy here)
Adjustable Gastric Banding (AGB): An inflatable band placed around the upper stomach restricts food intake. This is a less invasive option, but its effectiveness may vary, and adjustments might be needed over time. (Illustration of adjustable banding here)
The choice depends on individual health, lifestyle, and risk tolerance. Thorough consultation is essential to establish the most suitable procedure.
Risk Assessment: Understanding the Potential Complications
Bariatric surgery, while transformative, carries inherent risks. Short-term risks can include bleeding, infections, and leaks at the surgical site. Long-term complications may involve nutrient deficiencies (requiring supplementation), gallstones, and dumping syndrome (rapid gastric emptying). Dr. David Lee, MD, PhD, from the Cleveland Clinic, notes, "While complications are relatively infrequent, open communication about their potential is vital in ensuring patients make fully informed decisions." A detailed discussion with your surgeon regarding individual risk profiles is crucial. Is it possible to quantify risk based on patient characteristics and procedure type? This would strengthen the decision-making process.
Long-Term Outcomes and Lifestyle Transformation
Sustained weight loss hinges on long-term lifestyle modifications. Dietary changes, regular physical activity, and consistent follow-up are essential. Supplementation is crucial, particularly after malabsorptive procedures. Continuous engagement with support groups or counseling can significantly enhance adherence to the post-operative plan and improve long-term outcomes. Are there specific success rate metrics linked to consistent post-operative support? This data would provide invaluable context for patients.
Insurance Coverage and Cost Considerations
Bariatric surgery's cost can be substantial. Insurance coverage varies significantly; hence, a pre-operative assessment of your policy is vital. Understanding the extent of coverage, co-pays, and deductibles is crucial in managing the financial implications. Exploring financing options may be necessary for some. A clear understanding of financial responsibilities empowers informed decision-making. What is the average cost of these procedures and associated care, and what are common insurance coverage scenarios? This information would help patients plan effectively.
Conclusion: Empowered Decision-Making
Low BMI weight-loss surgery requires careful consideration of multiple factors. This guide provides a foundation for informed decision-making. Extensive discussion with a qualified bariatric surgeon, psychologist, and financial advisor significantly enhances the planning and decision-making process. Prioritizing open communication and a thorough understanding of the procedure, risks, and post-operative requirements sets the stage for patient empowerment and success.
Resources
- American Society for Metabolic and Bariatric Surgery (ASMBS): [Insert Link Here]
- National Institutes of Health (NIH): [Insert Link Here]
Key Takeaways:
- Eligibility for low BMI bariatric surgery extends beyond BMI, encompassing comorbidities and overall health.
- Numerous surgical options cater to diverse needs and risk profiles, necessitating individualized assessment.
- Post-surgical success depends significantly on long-term lifestyle commitment and ongoing care.